Main navigation
Click Below to View Our Laboratory and Screening Services
Labs and Screening
Carver Lab for Molecular Diagnosis
The John and Marcia Carver Nonprofit Genetic Testing Laboratory
The John and Marcia Carver Nonprofit Genetic Testing Laboratory is dedicated to providing non-profit genetic testing for rare eye diseases to meet a societal need. Most of the diseases that we study are so rare that commercial tests would be unlikely to be viable for the long term. As a result, many individuals affected with these diseases and their families would have little access to molecular information. Genes that are available for screening by the Carver Laboratory have previously been extensively studied in the research laboratories of Dr. Stone and Dr. Sheffield. By incorporating this research information into the design of the tests, the laboratory is able to offer genetic tests that provide the most clinically relevant information to patients and their families while keeping the tests affordable.
There is something you can do! For details about the laboratory and services, please visit The Carver Laboratory site.
Ophthalmic Electrophysiology (Electroretinography-ERG)
Electrophysiology testing includes a battery of tests which can be used to provide information about the visual system beyond the standard clinical examination of the eye. Electroretinography (ERG) and Electro-oculography (EOG) are two of the tests conducted in the Ophthalmic Electrophysiology Laboratory. The primary objective of the electrophysiologic examination is to assess the function of the visual pathway from the photoreceptors of the retina to the visual cortex of the brain. Information obtained from these diagnostic tests helps establish the correct diagnosis or may rule out related ophthalmic diseases.
Electrophysiologic testing is useful in diagnosing a variety of inherited retinal and optic nerve diseases, toxic drug exposure, inflammatory conditions, intraocular foreign bodies, and retinal vascular occlusions. Electrophysiologic testing is performed most often in large referral centers which have expertise in obtaining and interpreting these data. The data are used in conjunction with the clinical examination and other tests (perimetry, dark adaptometry) to establish a correct diagnosis.
The Electrophysiology Service at the University of Iowa specializes in:
- Standardized full-field electroretinography (ERG)
- Multifocal electroretinography (mfERG or mERG)
- Dark adaptometry
Physicians:
Arlene V. Drack, MD, Medical Director
Dr. Drack's Lab Site (patient and research information)
Staff:
Wanda Pfeifer, OC(C),COMT, Coordinator, (319) 356-1985, Wanda-Pfeifer@uiowa.edu
For more detailed information or consultation call 319-356-1985.
Full Field Electroretinography (ERG)
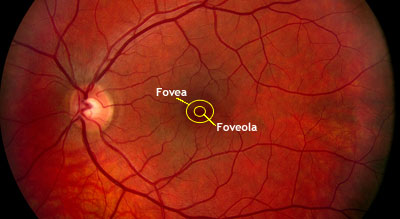
Full Field Electroretinography (ERG) is a test used to detect abnormal function in the retina (the light-detecting portion of the eye). Specifically, this test examines the function of the light-sensitive cells of the eye (the photoreceptors), and several other cells that process these light signals before they are sent to the brain. Photoreceptors are specialized nerve cells in the eye that are sensitive to light. There are two types of photoreceptors in the human eye: rods and cones. Cones provide central high-acuity vision used for reading and are also color vision. There are 6 to 7 million cones in the retina, of which about 650,000 are concentrated in the foveola for central vision. Rods provide vision in dim light. There are about 120 million rods in the retina, of which none are located in the foveola.
During the ERG test, the photoreceptors produce tiny amounts of electricity in response to brief flashes of light. If we know exactly how much light enters the eye, and how much electrical response is generated, we can figure out how well the rods and cones are working. The differences in responses are analyzed to differentiate diseases which affect the rods from those which affect the cones or other cells in the retina.
To detect the electrical response of both the rods and the cones, special electrodes are placed on the surface of the eye. There are several types of electrodes; the type of electrode used will depend on the type of test being performed, the age of the patient, and the suspected condition.
How is an ERG done?
The patient assumes a comfortable position (lying down or sitting up). Usually the patient's eyes are dilated beforehand with standard dilating eye drops.
The patient will be asked to sit in the dark for 20 minutes. The patient may have someone sit with them or they may listen to music, but they will not be able to use any device that will emit a light. This allows the eyes to adjust to the darkness so that the function of the rod photoreceptors can be examined. After sitting in the dark, the technician will place numbing drops in the eyes. The patient is asked to look up, and an electrode is gently placed on each eye. Some electrodes are contact lenses with small wires attached; others are fine threads that lay across the surface of the eye. An additional electrode is placed on the forehead.
The test is painless. However, the electrode that rests on the eye may feel a little like an eyelash is in the eye. This sensation may persist up to several hours following completion of the ERG. One should not rub the eyes for at least an hour after an ERG (or any test in which the cornea has been numbed), to avoid scratching the cornea.
Flashes of light are used to stimulate the retina. The first light is so dim that only the rods respond. The response is sensed by the electrode, amplified, and displayed on a computer screen. The intensity of the testing light is progressively increased. We refer to this as the dark adapted phase and this part of the test may take 10 to 15 minutes.
We also record responses from the eye in the light adapted state. This is done by having the patient view a medium – bright light for 10 minutes. This light suppresses the rods and isolates cone function. Cone function is recorded in response to another series of flashes. In another test of cone function, a light flickering at 30 flashes per second is used as the stimulus. Rods are unable to respond to light flickering at such a fast frequency, so cone photoreceptors are selectively tested. We refer to this portion of the ERG testing as the light adapted phase, and this part of the test may take 10 to 15 minutes.
How to prepare for the test
No special preparation is necessary for this test. We ask that you do not wear any eye make-up the day of testing.
What is a normal outcome for an ERG?
A normal ERG contains an a-wave (initial negative deflection) followed by a b-wave (positive deflection). The leading edge of the a-wave is produced by the photoreceptors, while the remainder of the wave is produced by a mixture of cells.
What does an abnormal ERG mean?
An abnormal ERG result suggests abnormal function of the retina which may be caused by a number of diseases of the retina. The results of the ERG will be discussed with your doctor.
ERG under anesthesia
An electroretinogram (ERG) can be performed in the operating room under general anesthesia in children who are too young to understand and perform the test in the clinic. Children will first be evaluated in the clinic by Dr. Arlene Drack. If it is determined that an ERG under anesthesia is necessary, a pre-operative elevation will be conducted which will determine the need for a further anesthesia work up. The ERG performed in the operating room is very similar to the ERG preformed in the clinic. The dark adaptation is done under anesthesia, and then both the dark adapted and light adapted responses are recorded. The ERG under anesthesia takes approximately 90 minutes to perform.
Multifocal Electroretinography (mfERG)
Multifocal techniques, in particular the multifocal ERG, are used in the diagnosis of ophthalmological diseases. The mfERG is a technique for assessing the local ERG from different regions of the retina. The mfERG is particularly valuable in cases in which the retina appears normal and it is difficult to distinguish between diseases of the retina and diseases of the optic nerve.
Electrical responses from the eye are recorded with an electrode just as in conventional ERG recording, but the special nature of the stimulus and analysis produces a more detailed map of where in the central retina ERG responses are normal or abnormal. This can help distinguish among different diseases.
For the routine mfERG, the retina is stimulated with a pattern of hexagons. The pattern will seem to flicker randomly, but each element follows a fixed, predetermined sequence called an ‘m sequence’. By correlating the continuous ERG signal with the on or off phases of each stimulus element, the focal ERG signal associated with each element is calculated.
How is the mfERG done?
As in full field ERG the patient assumes a comfortable seated position. Usually the patient's eyes are dilated beforehand with standard dilating eye drops. The technician will place a numbing drop in the eye. The patient is asked to look up, and an electrode is gently placed on the eye. An additional electrode is placed on the forehead. The eye not being tested is covered with a black eye patch.
The patient will be asked to continuously look at an ‘X’ located in the center of a monitor. The monitor will display a flashing hexagon pattern for 30 seconds, and then stop. This will be repeated 8 times for each eye. The test will take approximately one hour to complete.
How to prepare for the test
No special preparation is necessary for this test. We ask that you do not wear any eye make-up the day of testing.
What is the outcome for a mfERG?
Data can be displayed in various ways, such as waveform traces or colored graphs. The results of the mfERG will be given to your doctor for analysis and may be discussed with you at a later date.
Dark Adaptometry (DA)
Dark adaptometry (DA) measures the eye’s ability to detect a dim light, a measure of rod photoreceptor function. Two values are measured: the dimmest light the eye can detect the dark adaptation threshold and the time it takes to detect a dim light after going from condition of bright light to darkness, dark adaptation curve. Dark adaptometry may be used in concert with other tests such and the ERG or mfERG.
How is the test done?
Dark Adaptation Curve
The test is performed in a dark room. The patient will hold a special light to their eye and look at a bright light for 1 minute. After 1 minute, the patient will be asked if they can see another dimmer light. The light will continue to be presented at regular intervals until it is seen. Once seen, the light will be dimmed more and the test will continue until the dimmest light is no longer seen. The time at which each light intensity is seen is documented and recorded on a graph. This test will take approximately 30 to 45 minutes to perform.
Dark Adaptation Threshold
This test is performed in a dark room, after the patient is asked to sit in the dark for 30 to 45 minutes. This allows the eyes to be their most sensitive for the light. A light is presented to the patient and its brightness is changed until the dimmest light that can be seen has been determined. This process usually takes 3-5 minutes.
Types of Electrodes
Burian-Allen Electrodes
Burian-Allen Electrodes are bipolar, reusable contact lens electrode with built-in lid speculum and lead wire. They are available in a number of sizes. We use these electrodes mainly on sedated patients.
DTL Plus Electrodes
DTL Plus Electrodes are disposable, mono-polar Silver-Nylon thread electrode with adhesive fasteners. This is our main electrode.
Eye Pathology Lab
Named for the late Professor Frederick C. Blodi, this facility provides diagnostic services and supports a wide variety of vision-related research projects.
The laboratory is a service of the Department of Ophthalmology and Visual Science. It is affiliated with part of the system of diagnostic laboratories in the Department of Pathology, a vital part of the University of Iowa Health Care.
Perimetry

Perimetry is the systematic measurement of visual field function (the total area where objects can be seen in the peripheral vision while the eye is focused on a central point). The two most commonly used types of perimetry are Goldmann kinetic perimetry and threshold static automated perimetry.
A visual field test (perimetry) will detect loss of peripheral vision and provide a map of that loss which will be helpful in diagnosing the cause of the loss.
The highly trained perimetrists at the University of Iowa measure peripheral vision to evaluate glaucoma, neurological diseases, and retinal diseases. They employ manual techniques (Goldmann perimetry) and computer-driven automated techniques (Humphrey and Octopus perimetry). In addition they use a laser scanning device to analyze the structure of the optic nerve (Heidelberg Retinal Tomography).
Matthew J. Thurtell, MBBS, MSc, is the director of this service.
Learn More about Past and Present Perimetry Methods at the IPS site.
Echography (Ultrasound)
Staff
Physicians
- H. Culver Boldt, MD, 319-353-6112, culver-boldt@uiowa.edu
Technicians
- Rodney Berry, 319-356-2901, rodney-berry@uiowa.edu
- Andrea Hoback, 319-356-2901, andrea-hoback@uiowa.edu
- Laura L. Warner, 319-356-2901, laura-warner@uiowa.edu
Ocular Echography
Light in the visible part of the spectrum has been used for millennia to examine the eye and diagnose ocular disorders. Since 1956, scientists have used high frequency sound waves, or ultrasound, to examine the eye and diagnose disorders that might not be visible using light. The interpretation of the reflections (or echos) of these ultrasound waves from ocular tissues is called ocular echography.
By definition, ultrasound waves have frequencies greater than 20 kHz (20,000 oscillations/sec), which is above the frequency which is audible to the human ear. The typical frequencies used in diagnostic ophthalmic ultrasound are in the range of 8 to 10 million oscillations/sec. The sound waves are produced by a small probe which is placed directly on the eye following the application of a topical anesthesia. The same probe is used to collect returning echos, and these echos are then processed to create an image of the globe. This painless, non-invasive technique can be easily performed in the clinic, at the patient's bedside, or in the operating room. In addition, ultrasound can readily be performed on children, often without sedation.
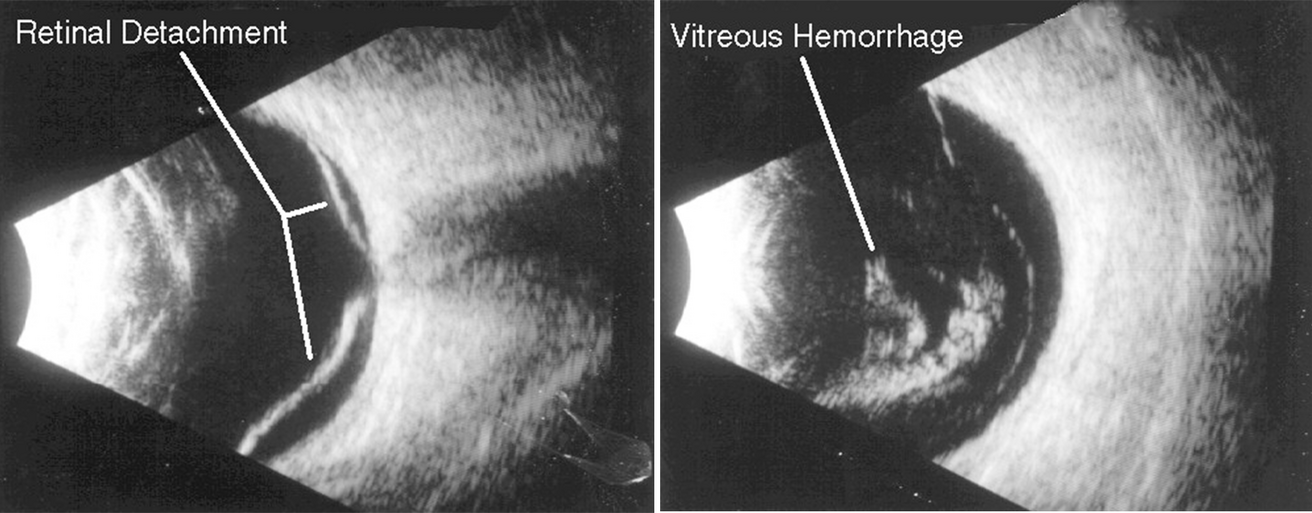
A major use of ocular echography is to examine the back of the eye in patients who have cloudy ocular media, such as cataract, corneal clouding, or blood in the vitreous fluid. B-scan echography uses a rapidly oscillating transducer to produce a 2 dimensional "slice" through the globe, similar to the image produced by a CT scan. However, the B-scan is far superior to CT images in detecting and distinguishing between the different structures in the eye. The echographic images are viewed on an oscilloscope, and movements of intraocular structures can be viewed in real time. Unlike CT, which uses potentially harmful ionizing radiation, echography utilizes high frequency sound waves at an intensity which appears to be very safe to tissues. One of the most frequent indications for ocular echography is to examine the retina in diabetic patients who have developed vitreous hemorrhage, to determine whether they have developed a potentially blinding condition called a retinal detachment.
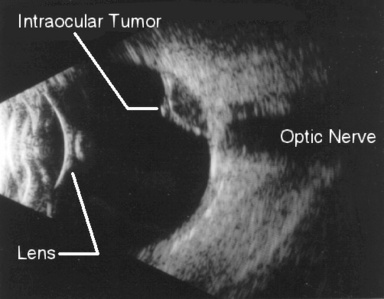
Ocular echography is very useful in differentiating between various intraocular tumors. A vital component of this examination involves the use of standardized A-scan echography, as developed by our own Dr. Karl Ossoinig. Dr. Ossoinig's techniques have vastly improved our ability to detect and differentiate intraocular disorders, and has allowed echographers to be able to compare and rely on the results of fellow investigators. A-scan echography is also frequently used by ophthalmologists to precisely measure the length on an eye prior to cataract surgery, to determine the strength of the lens implant to be placed in the eye at the time of cataract surgery.
Orbital Echography
Echography is also very useful in examining the soft tissue structures surrounding the eye. Infections, tumors, congenital abnormalities, inflammatory disease, traumatic disorders, and many other problems can be reliably diagnosed and followed using echography. In addition to standardized A-scan and B-scan instruments, a doppler instrument is also useful in examining the orbit, to listen for blood flow. The use of these instruments in combination with meticulous examination techniques as devised by Dr. Ossoinig has evolved into what is known today as Standardized Echography.
The Ophthalmic Echography Service evaluates about 75 patients a month, and is a resource used extensively by the other ophthalmic services at the University of Iowa as well as by ophthalmologists from Iowa and the surrounding states.
KidSight

Dedicated to enhancing the early detection and treatment of vision impairments in young children in Iowa communities through screening and public education.
Iowa KidSight is a joint project of the Lions Clubs of Iowa and the Department of Ophthalmology & Visual Sciences at the University of Iowa Health Care Stead Family Children’s Hospital.
Request a Free Vision Screening (ages 6 months to kindergarten)
Iowa Lions Eye Bank

The Iowa Lions Eye Bank is a non-profit service organization dedicated to the restoration and preservation of sight through the recovery, processing and distribution of human ocular tissue for transplantation and research, primarily in Iowa, but also throughout the world. The Iowa Lions Eye Bank is affiliated with the Department of Ophthalmology and Visual Sciences at the University of Iowa Health Care in Iowa City, Iowa.
Visitors are always welcome, and tours can be arranged for individuals or groups. Call 319-335-4888 or 1-866-HELP-SEE (toll free) with questions, tour requests, or club programs.
Pupillography
Pupillography is a test that measures the response of the pupils to a standardized brief light stimulus.
Dr. Randy H. Kardon directs the Pupillography Laboratory at the University of Iowa and conducts clinical and research evaluations of pupillary movements of the iris in health and disease. In addition, the computerized infrared instrumentation is equipped to record dynamic eye movements, and eyelid movements in addition to the dynamics of pupil movements.
